In vitro fertilization (IVF) is a technique that seeks to bring eggs and sperm together in the laboratory setting so that these may form embryos that can be transferred to the mother's uterus. Eggs can be fertilized by conventional IVF or through a process known as intracytoplasmic sperm injection (ICSI).
What does it involve?
1. Ovarian stimulation
Controlled ovarian stimulation involves having injections so that, rather than producing just one egg (as happens naturally each month), the ovaries produce more eggs that are viable for fertilization so as to increase the number of embryos produced.
The treatment lasts between 10 and 20 days depending on the protocol used. Clinical monitoring is performed during this time, consisting of assessments of hormone levels in the blood and ultrasound monitoring of follicle development, both aiming to check that the follicles are growing and developing properly.
2. Egg retrieval
Once we confirm that most of the follicles are at least 19–21 mm in size, the induction phase is brought to a close, and an injection is given subcutaneously to induce oocyte maturation. This takes place some 36 hours before egg retrieval.
The retrieval procedure is done on an outpatient basis so the patient does not need to stay overnight in the hospital. Puncture or retrieval takes place in the operating room while the patient is sedated so that she feels no discomfort.
Using a microscope, the embryologist will identify the oocytes that have been gathered during the procedure, and then these will be isolated and classified according to how far along they are in the maturation process. During this second phase we will need to have a sperm sample (from the partner or a donor) so that it can be prepared for insemination at a later point.
3. Fertilization
Once we have the eggs and sperm, the two are joined together so that fertilization may take place.
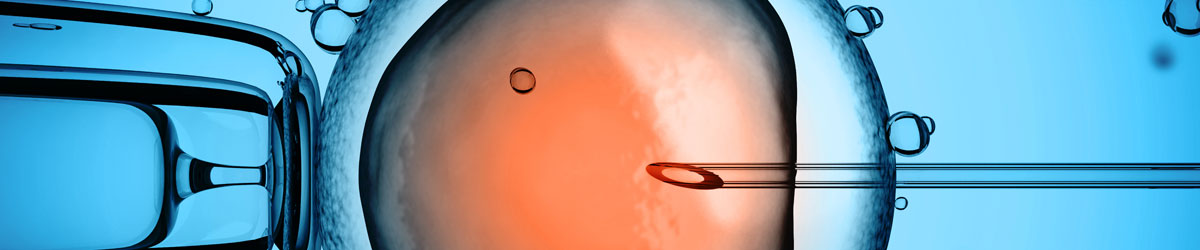
This process can be done using conventional IVF, which consists of placing an egg and a high quantity of viable sperm (about 250,000/ml) together in a petri dish, or, alternatively, through ICSI, which involves injecting a single live sperm into the egg. These are then stored in an incubator at 37°C in an atmosphere with a mix of gases and humidity level that are similar to those of the human body.
ICSI might be used, which consists of inserting a single live sperm into the egg. These are then stored in an incubator at 37°C in an atmosphere that has a similar mix of carbon dioxide and a humidity level to those of the human body.
The embryos created are tracked for morphology and ability to undergo cell division.
4. Embryo transfer
During this phase, viable embryos are inserted through the cervix and deposited at a distance of about 1.5 cm from the uterine fundus. This is done using a special catheter specifically used for embryo transfer. The number of embryos to be transferred depends on the patient's age, the number of unsuccessful previous attempts, and the doctor's assessment.
The patient does not need to take painkillers, as the procedure is quick and painless. It is, however, performed in an operating room located near the reproduction laboratory.
The patient and medical team together will decide whether a period of rest is necessary.
Over the next few days, it is often necessary for the patient to be treated with progesterone either vaginally or subcutaneously, and in some cases the patient will need to receive oral, vaginal, or transdermal estrogen.
A pregnancy test is done 12 to 14 days after the transfer. With a urine-based pregnancy test, the patient can find out the results of the test in privacy, creating a more appropriate setting to take in the result and manage its emotional implications.
5. Embryo vitrification
After the transferral process has concluded, all quality, viable embryos that have not been transferred are vitrified so they may be used in a later cycle without the need for further ovarian stimulation.
When is it recommended?
With your partner's sperm
-
For women with moderate or severe endometriosis
-
Failure of artificial insemination
-
In women with blocked fallopian tubes or adhesions
-
Moderate-to-severe abnormalities in a male partner
-
Egg donation techniques
With sperm from a donor
-
Single mother-to-be or two same-sex parents
-
Repeated failure of insemination with sperm from a male partner
-
Severe abnormalities in a male partner
-
Repeated implantation failure
How effective is it?
- ICSI fertilization has a similar effectiveness to IVF.
- The rate of pregnancy obtained, which on average is over 50% per cycle, is largely dependent on the woman's age and the number of embryos transferred.
© 2024 Quirónsalud - All rights reserved